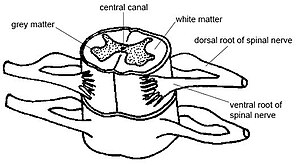
- Image via Wikipedia
The following is deep and steeped with big words. However, the words also include definitions, so don’t let it stop you from reading. It’s written by a mentor of mine and I wanted you to get a much fuller and deeper understanding of what chiropractic is and why you NEED to know!
If you have any questions go to www.nevadachiro.com or call 565-7474.
A Four-Dimensional Model of Vertebral Subluxation
By Christopher Kent, DC, Esq.
Vertebral subluxation represents the heart and soul of chiropractic, yet to many chiropractors, it remains a clinical conundrum. I believe that the controversy and confusion surrounding the chiropractic concept of vertebral subluxation is due, in part, to the lack of an operational definition compatible with most techniques.
A review of models of vertebral subluxation has been published elsewhere.1 However, regardless of the elegance of a theoretical model, it must be capable of being operationalized if it is to be used to develop clinical strategies. The four-dimensional model was developed as an initial step in the operational definition of vertebral subluxation. It incorporates traditional chiropractic constructs and serves as a bridge to contemporary technology.
The First Dimension
The traditional safety-pin cycle (SPC) consists of the transmission of afferent information from the tissue cell (periphery) to the brain cell (epiphery) on one side, and on the efferent side, from brain cell to tissue cell.2 In the 4-D model, the first dimension is dysafferentation, representing the afferent portion of the SPC. Aberrant afferent input to the CNS may result in qualitatively and/or quantitatively inappropriate responses to changes in the internal or external environment.1 In the contemporary jargon of the computer industry, there is “garbage in – garbage out.” Dr. Fred Barge, in his book One Cause, One Cure, stated that the cause of disease is “The body’s inability to comprehend itself and/or its environment.”3 Such “comprehension” is dependent upon interference-free afferent input.
Dye4 quoted remarks, attributed to B.J. Palmer in August 1935, which express this concept, noting the result of an adjustment: “[T]he restoration of the normal transmission of mental impulse supply from its point of origin within the brain to its point of expression in the diseased part of the body, or vice versa, that the Innate Intelligence within the brain may receive correct, accurate, exact messages as to the external conditions existing at the periphery so that it may direct either the necessary reparative forces or the necessary cooperative forces from that the tissues may be repaired or that the organ or structure may be properly directed that it may perform the normal functioning desired and indicated by the incoming message from me part without.”
The authors of the remarkable book Segmental Neuropathy, published by Canadian Memorial Chiropractic College, proposed the concept of a “neural image,” dependent upon the integrity of neural receptors and afferent pathways. This “neural image” is a representation of the organism’s perception of the external and internal environment. If afferent input is compromised, efferent response may be qualitatively and quantitatively compromised.5
The clinical implications of aberrant or suboptimal afferent go beyond short-term homeostatic regulation. Dysafferentation may result in anatomical and functional changes in the brain itself. Merzenich6 noted, “The brain was constructed to change.” This challenge to the conventional world view that the mature adult brain is stable and unchanging, the only exception being the death of brain cells, has profound implications for the chiropractor.
Gage7 stated, “Researchers first demonstrated that the central nervous systems of mammals contain some innate regenerative properties in the 1960s and 1970s, when several groups showed that axons, or main branches, of neurons in the adult brain and spinal cord can regrow to some extent after injury.” The ability of the brain to change both anatomically and functionally is known as neuroplasticity. Three types have been described:8
- Experience-independent plasticity refers to changes which are not the result of environmental changes or influence.
- Experience-expectant plasticity occurs when the brain uses input from the external environment to effect normal developmental changes in its structure.
- Experience-dependent plasticity is when a modification to the internal or external environment produces change in a feature of the brain.
Holloway6 explained how the brain reconfigures itself and the implications of doing so: “Change the input, be it a behavior, a mental exercise … or a physical skill and the brain changes accordingly. Magnetic resonance imaging machines reveal the new map: different regions light up … [T]he brain can be extensively remodeled throughout the course of one’s life, without drugs, without surgery. Regions of the brain can be taught to do different tasks if need be … This sort of thing will be a part of normal future life … healing plasticity can be driven by behavior.”
The 2nd-4th Dimensions
The remaining three dimensions represent the efferent portion of the safety-pin cycle. Each component may be reliably measured. These measurements provide objective evidence concerning manifestations of vertebral subluxation. The three components are:
- Dyskinesia. Dyskinesia refers to distortion or impairment of voluntary movement.9 Spinal motion may be reliably measured using inclinometry.10 Alterations in regional ranges of motion are associated with vertebral subluxation.11
- Dysponesis. Dysponesis is abnormal involuntary muscle activity. Dysponesis refers to a reversible physiopathologic state, consisting of errors in energy expenditure which are capable of producing functional disorders. Dysponesis consists mainly of covert errors in action potential output from the motor and premotor areas of the cortex and the consequences of that output. These neurophysiological reactions may result from responses to environmental events, bodily sensations, and emotions. The resulting aberrant muscle activity may be evaluated using surface electrode techniques.12 Typically, static surface electromyography (SMEG) with axial loading is used to evaluate innate responses to gravitational stress.13
- Dysautronomia. The autonomic nervous system regulates the actions of organs, glands, and blood vessels. Acquired dysautonomia may be associated with a broad array of functional abnormalities.14-19 Autonomic dystonia may be evaluated by measuring skin temperature differentials.20 Uematsu, et al., determined normative values for skin temperature differences based upon asymptomatic “normal” individuals. The authors stated, “These values can be used as a standard in assessment of sympathetic nerve function, and the degree of asymmetry is a quantifiable indicator of dysfunction … Deviations from the normal values will allow suspicion of neurological pathology to be quantitated and therefore can improve assessment and lead to proper clinical management.”21 Skin temperature differentials are associated with vertebral subluxation.22 Autonomic tone and balance may also be evaluated by measuring heart rate variability.23
This four-dimensional model may be used with any technique which has, as its objective, the detection, management or correction of vertebral subluxation. Correction or reduction of vertebral subluxation facilitates the restoration of proper tone throughout the nervous system. Alterations in the tone of the somatic system may be objectively evaluated using surface EMG. Altered autonomic tone may be evaluated using skin temperature measurements. Changes in ranges of motion may be measured to assess dyskinesia. Such objective assessments have the potential to make chiropractic the dominant strategy of 21st century health care.
References
- Kent C. Models of vertebral subluxation: a review. Journal of Vertebral Subluxation Research, 1996;1(1):11.
- Stephenson RW. Chiropractic Textbook. The Palmer School of Chiropractic: Davenport, IA. 1948 edition, page 9.
- Barge FH. One Cause, One Cure. LaCrosse, WI, 1990.
- Dye AA. The Evolution of Chiropractic. Published by A.A. Dye, DC: Philadelphia, 1939, page 266.
- Segmental Neuropathy. Canadian Memorial Chiropractic College. Toronto, Ontario. No date. Presumed to be written in the 1960s primarily by H.M. Himes and A. Peterson.
- Holloway M. “The Mutable Brain.” Scientific American, 2002;289(3):79.
- Gage FH. “Brain, Repair Yourself.” Scientific American, 2002;289(3):47.Neuroplasticity. PowerPoint lecture. www.snl.salk.edu/~nikoosh/Lecture_5.ppt
- Dorland’s Pocket Medical Dictionary., 25th Edition. WB Saunders Company, 1995.
- Saur PM, Ensink FB, Frese K, et al. Lumbar range of motion: reliability and validity of the inclinometer technique in the clinical measurement of trunk flexibility. Spine, 1996;21(11):1332.
- Blunt KL, Gatterman MI, Bereznick DE. Kinesiology: An Essential Approach Toward Understanding the Chiropractic Subluxation. Chapter 11 in Gatterman MI (ed): Foundations of Chiropractic Subluxation. Mosby: St. Louis, MO, 1995.
- Whatmore GB, Kohi DR. Dysponesis: a neurophysiologic factor in functional disorders. Behav Sci, 1968;13(2):102.
- Kent C. Surface electromyography in the assessment of changes in paraspinal muscle activity associated with vertebral subluxation: a review. Journal of Vertebral Subluxation Research, 1997;1(3):15.
- Backonja M-M. Reflex sympathetic dystrophy/sympathetically mediated pain/causalgia: the syndrome of neuropathic pain with dysautonomia. Seminars in Neurology, 1994;14(3):263.
- Goldstein DS, Holmes C, Cannon III RO, et al. Sympathetic cardioneuropathy in dysautonomias. New Engl J Med, 1997;336(10):696.
- Vassallo M, Camilleri M, Caron BL, Low PA. Gastrointestinal motor dysfunction in acquired selective cholinergic dysautonomia associated with infectious mononucleosis. Gastroenterology, 1991;100(1):252.
- Baron R, Engler F. Postganglionic cholinergic dysautonomia with incomplete recovery: a clinical, neurophysiological and immunological case study. J Neurol, 1996;243:18.
- Soares JLD. Disautonomias. Acta Medica Portuguesa, 1995;8(7- 8):425. Written in Portuguese. English abstract.
- Stryes KS. The phenomenon of dysautonomia and mitral valve prolapse. J Am Acad Nurse Practitioners, 1994;6(1):11.
- Korr IM. The Collected Papers of Irvin M. Korr. American Academy of Osteopathy: Indianapolis, IN, 1979.
- Uematsu S, Edwin DH, Jankel ER, et al. Quantification of thermal asymmetry. J Neurosurg, 1988;69:552.
- Kent C, Gentempo P. “Instrumentation and Imaging in Chiropractic: A Centennial Retrospective.” Today’s Chiropractic, 1995;24(1):32.
- Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Circulation, 1996;93:1043-1065.