Journal of Human Hypertension 2007 (May); 21 (5): 347–352 ~ FULL TEXT
Bakris G, Dickholtz M, Meyer PM, Kravitz G, Avery E, Miller M, Brown J, Woodfield C, Bell B
Department of Preventive Medicine, Rush University Hypertension Center, Chicago, IL, USA
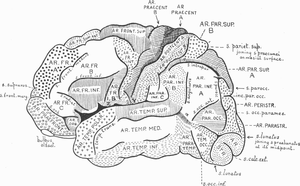
Anatomical abnormalities of the cervical spine at the level of the Atlas vertebra are associated with relative ischaemia of the brainstem circulation and increased blood pressure (BP). Manual correction of this mal-alignment has been associated with reduced arterial pressure. This pilot study tests the hypothesis that correcting mal-alignment of the Atlas vertebra reduces and maintains a lower BP. Using a double blind, placebo-controlled design at a single center, 50 drug naive (n=26) or washed out (n=24) patients with Stage 1 hypertension were randomized to receive a National Upper Cervical Chiropractic (NUCCA) procedure or a sham procedure. Patients received no antihypertensive meds during the 8-week study duration. The primary end point was changed in systolic and diastolic BP comparing baseline and week 8, with a 90% power to detect an 8/5 mm Hg difference at week 8 over the placebo group. The study cohort had a mean age 52.7+/-9.6 years, consisted of 70% males. At week 8, there were differences in systolic BP (-17+/-9 mm Hg, NUCCA versus -3+/-11 mm Hg, placebo; P<0.0001) and diastolic BP (-10+/-11 mm Hg, NUCCA versus -2+/-7 mm Hg; P=0.002). Lateral displacement of Atlas vertebra (1.0, baseline versus 0.04 degrees week 8, NUCCA versus 0.6, baseline versus 0.5 degrees , placebo; P=0.002). Heart rate was not reduced in the NUCCA group (-0.3 beats per minute, NUCCA, versus 0.5 beats per minute, placebo). No adverse effects were recorded. We conclude that restoration of Atlas alignment is associated with marked and sustained reductions in BP similar to the use of two-drug combination therapy.
From the Full-Text Article:
Discussion
The findings of this pilot study represent the first demonstration of a sustained BP lowering effect associated with a procedure to correct the alignment of the Atlas vertebra. The improvement in BP following the correction of Atlas misalignment is similar to that seen by giving two different antihypertensive agents simultaneously. [11, 12] Moreover, this reduction in BP persisted at 8 weeks and was not associated with pain or pain relief or any other symptom that could be associated with a rise in BP.
Other studies support the notion that changes in the cerebral circulation that is related to the position of the Atlas vertebra can affect BP. Coffee et al. [9] reviewed MR images and demonstrated a significant association between pulsatile arterial compression of the ventrolateral medulla and presence of hypertension. They concluded that subjects with hypertension should have an evaluation of their posterior fossa for evidence of anatomic abnormalities. [9 ] In fact, data linking changes in Atlas anatomy and posterior fossa circulatory changes associated with hypertension date back more than 40 years and are reviewed by Reis. [4]
The mechanism as to why this improvement in BP occurs is unknown and cannot be determined by this study. What is clear is that a significant change in sympathetic tone is probably not a major contributing mechanism as heart rate was not significantly changed. The data presented, however, raises a number of important questions including: (a) how does misalignment of C1 affect hypertension? (b) If there is a cause and effect relationship between C1 misalignment and hypertension is malposition of C1 an additional risk factor for the development of hypertension?
What is clear is that misalignment of the Atlas vertebra can be determined by assessment of the alignment of the pelvic crests. This should be considered in those who have a history of hypertension and require multiple medications for treatment. Additionally, it should be considered in those with refractory hypertension and a history of neck injuries, independent of the presence of pain. Note that pain was not present in any of the patients randomized in this study.
As discussed in the Methods section of this paper, techniques are now available to screen for atlas misalignment. This type of screening should be the responsibility of the primary care physician and should be performed on patients who have a history of head and neck trauma even if it is deemed insignificant. Those patients who present with pain related to head and neck trauma should not be screened. At a time when the prevalence of hypertension is increasing and its control more difficult due to a variety of factors, linking the correction of C1 misalignment to the subsequent lowering of BP may represent an important advancement in the screening of such patients.
This pilot study has limitations including the fact that it was dependent on the skill of one practitioner to do the manipulation. It was designed, however, to test the concept that nonsurgical manipulation can alleviate elevations in BP, thus it cannot be generalized until confirmed in a larger trial, which is being planned.
What is known about this topic:
- The relationship between hypertension and presence of circulatory abnormalities in the area around the Atlas vertebra have been known for more than 40 years [3–5]
- Recent studies by Akimura et al. [8] noted compression of the ventrolateral branches of the vertebral artery in the area around the Atlas vertebra in 90.6% hypertensive cases
- Thus, alterations in Atlas anatomy can generate changes in the vertebral circulation that may be associated with elevated levels of blood pressure
What does this study add
- This pilot study provides evidence that nonsurgical interventions to align the Atlas vertebra provide long-term amelioration in blood pressure
- It provides the first nonsurgical approach to alleviating elevations in blood pressure
References
1 Randomization of patients Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure
Hypertension 2003; 42: 1206–1252
2 Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000
JAMA 2003; 290: 199–206
3 The C1 area of the brainstem in tonic and reflex control of blood pressure. State of the art lecture
Hypertension 1988 (Feb); 11 (2 Pt 2): 18-13
4 The brain and hypertension: reflections on 35 years of inquiry into the neurobiology of the circulation
Circulation 1984; 70: III31–III45
5 Two specific brainstem systems which regulate the blood pressure
Clin Exp Pharmacol Physiol 1975; 12(Suppl 2): 179–183
6 Neurogenic hypertension: etiology and surgical treatment. I. Observations in 53 patients
Ann Surg 1985; 201: 391–398
7 Microvascular decompression in the treatment of hypertension: review and update
Surg Neurol 2001; 55: 2–10
8 Essential hypertension and neurovascular compression at the ventrolateral medulla oblongata: MR evaluation
AJNR Am J Neuroradiol 1995 (Feb); 16 (2): 401-5
9 Arterial compression of the retro-olivary sulcus of the medulla in essential hypertension: a multivariate analysis
J Hypertens 2005 (Nov); 23 (11): 2027-31
10 Arterial compression of the retro-olivary sulcus of the ventrolateral medulla in essential hypertension and diabetes
Hypertension 2005; 46: 982–985
11 Combination drug treatment for hypertension with nondiabetic renal disease
Curr Hypertens Rep 2005; 7: 358–359
12 Achieving goal blood pressure in patients with type 2 diabetes: conventional versus fixed-dose combination approaches
J Clin Hypertens 2003; 5: 202–209














 In their study, the researchers identified Blue Cross Blue Shield of Tennessee members with an LBP claim based on the presence of any of the following
In their study, the researchers identified Blue Cross Blue Shield of Tennessee members with an LBP claim based on the presence of any of the following 

