by Howard Loomis, D.C.
Before beginning this discussion, I wish to point out that current diagnosis of this seemingly pandemic condition is done without physical examination or objective testing. Recommendation of antacids, proton-pump inhibitors, and histamine antagonists, thus canceling normal digestion in the stomach, can only lead to chronic degenerative conditions.
GERD is a condition that is described as occurring when the acidified liquid contents of the stomach back up into the esophagus. This includes not only stomach acid, but pepsin as well and may even include bile that has backed-up into the stomach from the duodenum. The liquid can inflame and damage the lining of the esophagus, if it is not protected by the mucosal lining. This is in and of itself not a disease.
The symptoms of uncomplicated GERD are heartburn, regurgitation, and nausea, but these symptoms only occur in a minority of patients. This statement requires some explanation.
Reflux of the stomach’s liquid contents into the esophagus occurs in most normal individuals. In fact, one study found that reflux occurs as frequently in normal individuals as in patients with a diagnosis of GERD. There are several mechanisms that prevent the symptoms from occurring:
- Most reflux occurs during the day when we are upright and refluxed liquid is more likely to flow back down into the stomach due to the effect of gravity.
- When awake we repeatedly swallow and each swallow carries any refluxed liquid back into the stomach. Also saliva contains bicarbonate and with each swallow it travels down the esophagus and neutralizes the small amount of acid that remains in the esophagus after gravity and swallowing have removed most of the liquid.
- At night while sleeping, gravity is not in effect, swallowing stops, and the secretion of saliva is reduced. Therefore, reflux that occurs at night is more likely to result in acid remaining in the esophagus longer and can cause damage to the esophagus.
Symptoms of Uncomplicated GERD
Heartburn
When acid refluxes back into the esophagus in patients with GERD, nerve fibers in the esophagus are stimulated. This nerve stimulation results most commonly in heartburn, the pain that is characteristic of GERD. Heartburn usually is described as a burning pain in the middle of the chest. It may start high in the abdomen or may extend up into the neck. In some patients, however, the pain may be sharp or pressure-like, rather than burning. Such pain can mimic heart pain or angina. In other patients, the pain may extend to the back.
Episodes of heartburn tend to happen periodically. This means that the episodes are more frequent or severe for a period of several weeks or months, and then they become less frequent or severe or even absent for several weeks or months. Nevertheless, medicine considers GERD to be a chronic condition and once treatment for GERD is begun it is continued indefinitely.
Regurgitation
Usually only small quantities of liquid reach the esophagus, and the liquid remains in the lower esophagus. At the upper end of the esophagus is the upper esophageal sphincter (UES). The upper esophageal sphincter is a circular ring of muscle that is very similar in its actions to the lower esophageal sphincter (LES). That is, it prevents esophageal contents from backing up into the throat. When small amounts of refluxed liquid and/or foods pass back through the UES and enter the throat, there may be an acid taste in the mouth. If larger quantities breach the UES, patients may suddenly find their mouths filled with the liquid or food.
Nausea
Nausea is uncommon in GERD. In some patients, however, it may be frequent or severe and may result in vomiting. In fact, in patients with unexplained nausea and/or vomiting, GERD is one of the first conditions suspected. It is not clear why some patients with GERD develop mainly heartburn and others develop mainly nausea.
The Causes of GERD
These include an abnormal lower esophageal sphincter, weak or abnormal esophageal contractions, hiatal hernia, and slow emptying of the stomach – BUT NOT EXCESS STOMACH ACID PRODUCTION, except in the rare Zollinger-Ellison Syndrome. A small number of patients with GERD do produce abnormally large amounts of acid, but this is uncommon and not a contributing factor in the vast majority of patients.
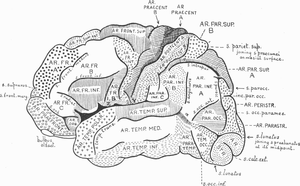
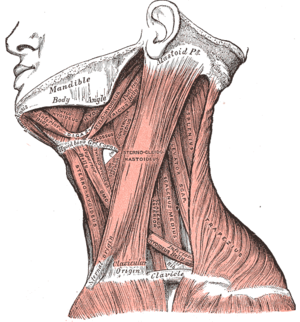
Lower esophageal sphincter (C3 to C5 and T4 to T9)
The action of the lower esophageal sphincter (LES) is the most important factor for preventing reflux. The LES is a specialized ring of muscle that surrounds the lower-most end of the esophagus where it joins the stomach. This muscle is active most of the time, contracting and closing off the passage from the esophagus into the stomach. When food or saliva is swallowed, the LES relaxes for a few seconds to allow the food or saliva to pass into the stomach, and then it closes again. Two abnormalities of the LES have been found in patients with GERD:
- The first is abnormally weak contraction of the LES, which reduces its ability to prevent reflux.
- The second is abnormal relaxations of the LES that do not accompany swallows and they can last up to several minutes.
These prolonged relaxations allow reflux to occur more easily. The transient LES relaxations occur in patients with GERD most commonly after meals when the stomach is distended with food.
Hiatal hernia
Hiatal hernias may contribute to reflux, but not necessarily. A majority of patients with GERD have hiatal hernias, but many do not AND many people have hiatal hernias but do not have GERD! There appear to be three reasons why a hiatal hernia can contribute to GERD:
- First, the LES is located at the same level where the esophagus passes from the chest through the diaphragm and into the abdomen. When there is a hiatal hernia, a small part of the upper stomach that attaches to the esophagus pushes up through the diaphragm. As a result, a small part of the stomach and the LES come to lie in the chest, and the LES is no longer at the level of the diaphragm. This means the barrier to reflux is equal to the sum of the pressures generated by the LES and the diaphragm.
- Second, a hiatal hernia produces a small pouch of stomach above the diaphragm. The sac is pinched off from the esophagus above by the LES and from the stomach below by the diaphragm. The sac traps acid that comes from the stomach and it is easier for the acid to reflux when the LES relaxes with a swallow or a transient relaxation.
- Finally, the esophagus normally joins the stomach obliquely, not straight on or at a 90-degree angle. Due to this oblique angle of entry, a flap of tissue is formed between the stomach and esophagus. This flap acts like a valve, shutting off the esophagus from the stomach and preventing reflux. When a hiatal hernia allows entry of the esophagus into the stomach the valve-like flap is distorted or disappears and it no longer can help prevent reflux.
Esophageal contractions
Swallowing is important in eliminating acid in the esophagus. Swallowing causes a ring-like wave of contraction of the esophageal muscles, which narrows the lumen of the esophagus. Peristalsis begins in the upper esophagus and travels to the lower esophagus. It pushes food, saliva, and whatever else is in the esophagus into the stomach. If the contraction is weak, refluxed acid cannot be pushed back into the stomach.
Abnormalities of contraction are found frequently in patients with GERD. In fact, they are found most frequently in those patients with the most severe GERD. Note that smoking also substantially reduces the clearance of acid from the esophagus. This effect continues for at least 6 hours after the last cigarette.
Delayed Emptying of the stomach
A minority of patients with GERD, about 20%, have been found to have stomachs that empty more slowly than normal after a meal. This slower emptying of the stomach prolongs the distention of the stomach with food after meals. Therefore, the slower emptying prolongs the period of time during which reflux is more likely to occur.
Hi. Dr. Swolensky again! If you have questions about this information please contact my office at www.nevadachiro.com or call (702) 565-7474.
















 In their study, the researchers identified Blue Cross Blue Shield of Tennessee members with an LBP claim based on the presence of any of the following
In their study, the researchers identified Blue Cross Blue Shield of Tennessee members with an LBP claim based on the presence of any of the following 